Kathy Hubble talks with Dr Ati Jhajj about her experience with the AH Program
Amelio Health Pain Program Details
Amelio Health is a digital therapeutic program that empowers participants with the knowledge to make informed choices about their recovery.
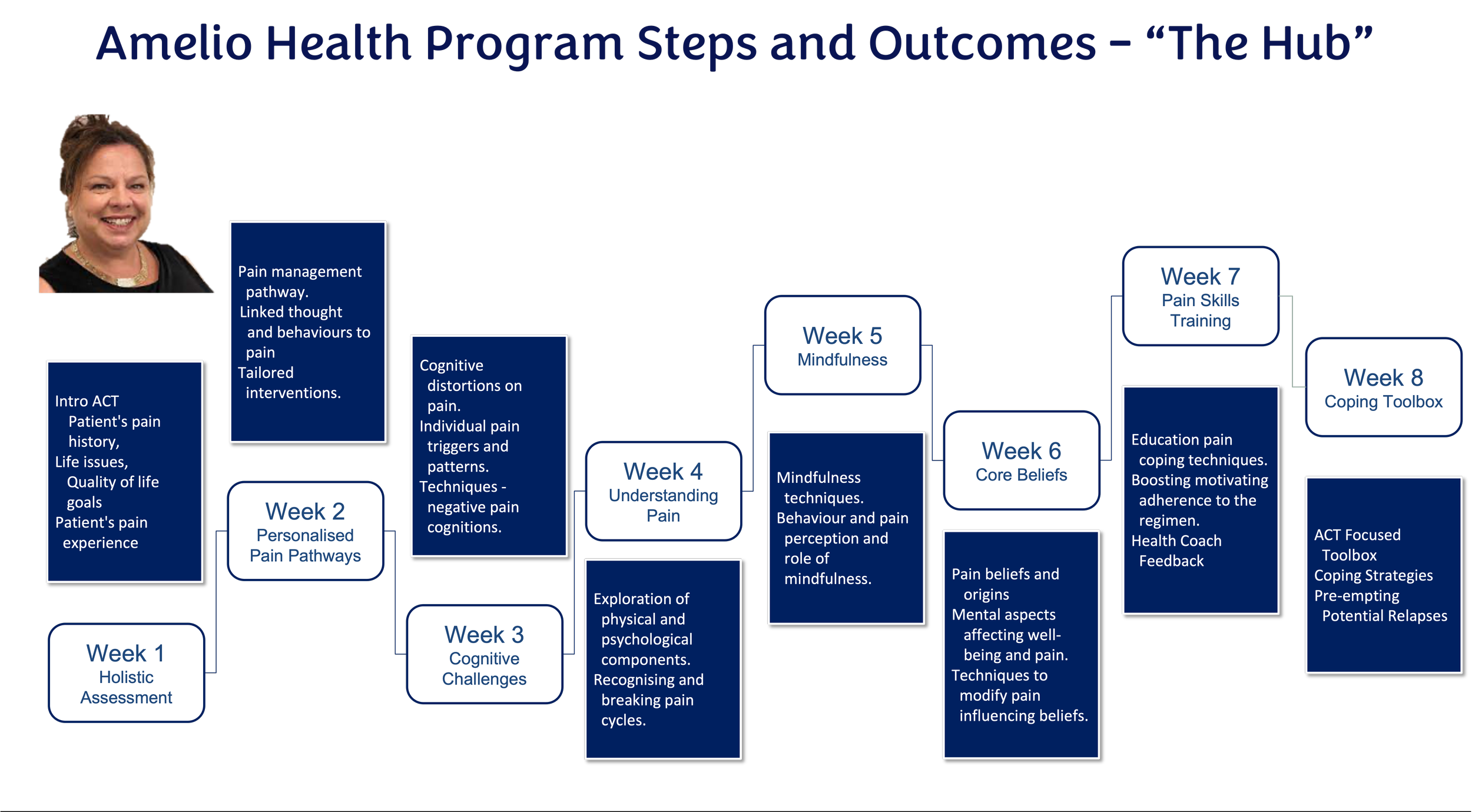
An eight-week intensive program, each module delivered in video format is embedded with core competencies from The International Association for the Study of Pain (IASP) and Bloom's Taxonomy of Learning Theory.
Data from biopsychosocial scores, wearables, and daily pain diaries is analysed and provided to live health coaches to drive behaviour change 24/7.
AI provides rules for closed-loop learning, predictive behaviour and decision support for Health Coaches, nudging at precise times for best outcomes.
AI provides automation of reporting to stakeholders. For the first time, data provides a 24/7 visual of how pain impacts a person's biopsychosocial life, and then AI drives precise nudging at the most opportune time.
“As a doctor, I found the programme revealed all the common gaps in pain treatment protocols and how by looking at the patient as a whole, we can achieve better outcomes. Seeing how real patients have found the Amelio Health platform helpful in getting their lives back is inspirational and prompts me to think about how I can do better for each patient. Kathy has such a wealth of knowledge, and if you treat any patients with chronic pain, you need to have a look at the way Amelio Health is revolutionising the care of their patients”
General Practitioner Dr Ati Jhajj from Sydney.
What advice is provided on people's well-being, and on what basis?
The outcome of the eight-week program is designed to equip each patient with an understanding of their health, including mental health and lifestyle factors that impact their ability to deal with their chronic pain.
The use of information from Fitbits and the feedback from AH coaches is focused on providing the tools for each patient to understand the changes they are making to things like diet, use of medications/treatments, activity levels, and sleep patterns that impact their perception of pain and how they can learn to control the factors that are influencing the pain they are experiencing.
The main differentiators of the program from other psychosocial programs include the patients' definition of outcomes important to them. These patient defined outcomes provide the basis for their participation in the program and their determination to make the necessary changes in their approach to their health and coping with chronic pain. We understand from each patient the important aspects of their lives where chronic pain is blocking and limiting their quality of life.
The program is tailored to assist each patient in making a range of lifestyle and health decisions equipped with their biofeedback (FitBit, video diaries and coaches) to provide a positive environment for behaviour and lifestyle change.
Fundamental Principles and Areas of Innovation
The program is exclusively online and is based on mindfulness principles to aid patients in reframing harmful thought patterns and accepting negative feelings as a normal part of life. Where cognitive behavioural therapies typically concentrate on short-term issues, AH combines CBT with Acceptance and Commitment Therapy to provide patients with the tools that can be integrated into their daily lives for the long term.
Our early research highlighted the need for positive feedback mechanisms for long-lasting change. Bloom's learning theory, wearable bio data loggers, personal mobile applications, and health coaches are all elements of positive feedback and ongoing monitoring to foster an environment for sustainable change in health and lifestyle outcomes.
Most importantly, the program is tailored to each participant's specific goals and can be accessed online and privately. The remote online nature of the program is ideal for patient privacy and AH is fully HIPPA compliant.
Patients find by participating in the program, individuals can experience benefits such as reduced stress, improved mental clarity, and better pain management. The program’s participants develop a daily mindfulness practice, improving their ability to manage pain and enhancing their overall well-being.
Further Reading
1. Lewin, A. M., M. Fearnside, R. Kuru, B. P. Jonker, J. M. Naylor, M. Sheridan, and I. A. Harris. 2021.
“Rates, Costs, Return to Work and Reoperation Following Spinal Surgery in a Workers’ Compensation
Cohort in New South Wales, 2010-2018: A Cohort Study Using Administrative Data.” BMC Health Services
Research 21 (1): 955
2. Deloitte Australia Access Economics. 2019. “The Cost of Pain in Australia | Deloitte Australia | Deloitte
Access Economics, Healthcare, Public Sector.” Deloitte Australia. April 3, 2019.
3. Chu, Larry F., Martin S. Angst, and David Clark. 2008. “Opioid-Induced Hyperalgesia in Humans: Molecular
Mechanisms and Clinical Considerations.” The Clinical Journal of Pain 24 (6): 479–96.
4. Di Donato, Michael, Ting Xia, Ross Iles, Rachelle Buchbinder, and Alex Collie. 2021. “Patterns of Opioid
Dispensing and Associated Wage Replacement Duration in Workers with Accepted Claims for Low Back
Pain: A Retrospective Cohort Study.” Pain, November. https://doi.org/10.1097/j.pain.0000000000002539.
5. Williams, A. C., M. K. Nicholas, P. H. Richardson, C. E. Pither, D. M. Justins, J. H. Chamberlain, V. R.
Harding, J. A. Ralphs, S. C. Jones, and I. Dieudonné. 1993. “Evaluation of a Cognitive Behavioural Programme for Rehabilitating Patients with Chronic Pain.” The British Journal of General Practice: The Journal of the Royal College of General Practitioners 43 (377): 513–18.
7.Feliu-Soler A, Montesinos F, Gutiérrez-Martínez O, Scott W, McCracken LM, Luciano JV. Current status of acceptance and commitment therapy for chronic pain: a narrative review. J Pain Res. 2018 Oct 2;11:2145-2159. doi: 10.2147/JPR.S144631. PMID: 30323649; PMCID: PMC6174685.
8.Lance M McCracken, professor of clinical psychology1, Lin Yu, lecturer in psychology2, Kevin E Vowles, professor of clinical health psychology3 2022 “New generation psychological treatments in chronic pain” BMJ 2022;376:e057212
9.Tefera YG, Gray S, Nielsen S, Collie A. Preoperative opioid use and postoperative return to work following spinal surgery in workers' compensation settings: A systematic review and meta-analysis. Int J Surg. 2024 Jan 4. doi: 10.1097/JS9.0000000000001035. Epub ahead of print. PMID: 38181114.